By Michael J. Baron, MD, MPH, DFASAM
Medical Director
Data is valuable in medicine because it empowers us to make informed evidence-based decisions that help enhance efficiency and improve outcomes. In the treatment world, outcome data is key – it shows the results of all the efforts made to bring an individual back to health and into long term, successful recovery.
Outcome data for addiction treatment measures the effectiveness of therapy and treatment. It goes beyond what was done, it also captures useful information such as recovery, sobriety, and return-to-use rates. This data is essential: it enables us to track progress and drives improvements in the recommendations we provide to our participants; it helps improve clinical decision-making and will help to adjust treatment plans when problems occur; it is also critical to help defend the use of expensive evaluations and long-term treatment.
Introduction
General outcome data for Professional Health Programs (PHPs) ranges from a few to many years old. We have always relied on this data but felt it was time to determine our own outcome data.
To remedy this problem, we embarked on an outcome study paid for in part by a grant awarded by the Opioid Abatement Council. We added a survey to query our active participants’ perception of which TMF services are most beneficial in maintaining sobriety. The OAC grant supported the implementation of the studies, as well as the PhD level biostatistician we retained to help manage both.
Our most significant challenge was data entry variability. In 2018, we changed from paper charts to an Electronic Health Record (EHR); however, our data was not easy to extract. It was polluted by too many drop-down choices, too many parameters, and inter-user variability. Before we could extract data for this study, we had to clean it, which took weeks of work by our clinical team. The resulting benefit was that it delineated our data entry problems and helped us implement more standardized data entry procedures.
Methods
Our study group was made up of 676 health professionals referred to the TMF and entered into our EHR over a five-and-a-half-year period, from December 2018 to July 2024. In that some participants had more than one Monitoring Agreement, we decided to report the data by using Participant Monitoring Agreements (PMAs) rather than Participants alone or Monitoring Agreements alone.
We dropped 406 participants from the group who never signed nor were asked to sign a PMA for various reasons, including being referred to non-TMF resources or solutions.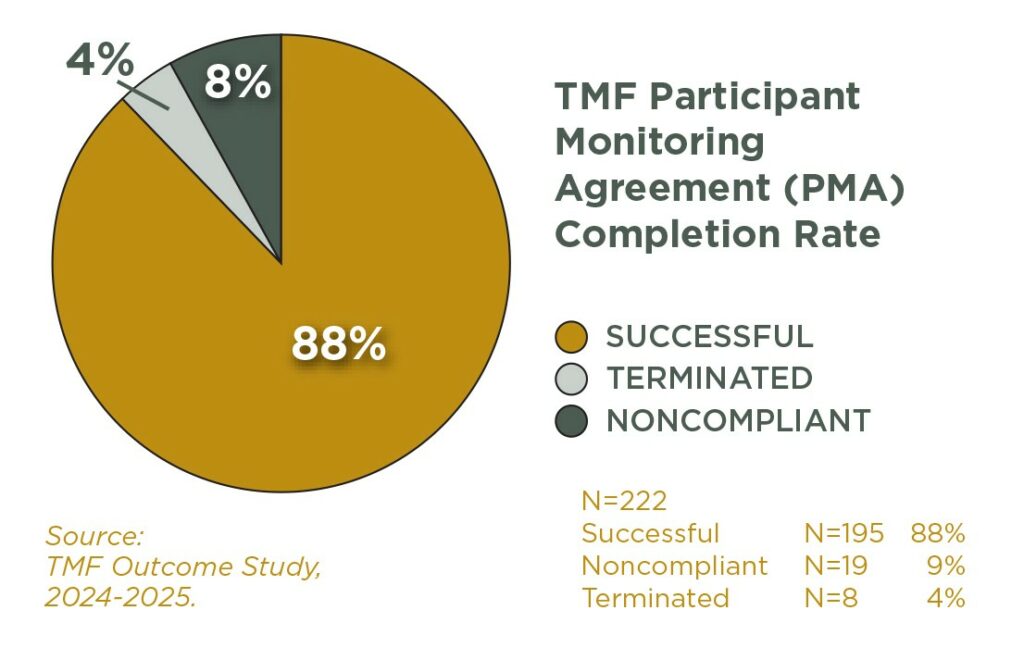
The remaining 270 were TMF participants who signed monitoring agreements (PMAs). We excluded participants whose agreements were ended for the following reasons: death (not due to substance use or suicide), retirement, released (agreements were ended when graduated medical school or residency and moved to another state), or voluntary withdrawal (due to lifetime monitoring requirements ended by the state or completion of a post-graduation Recovery Maintenance Agreement).
That left 222 participants who had signed PMAs. Of those, 195 PMAs (87%) were successfully completed. Eight (4%) were closed due to revocation of the participant’s medical license, which meant they could no longer be monitored. 19 participants (9%) could no longer be monitored because they were non-compliant. Three participants initially in the non-compliant group went on to successfully complete a monitoring agreement, so they were counted in both groups.
Results
Overall, 87% of our Participant Monitoring Agreements were successfully completed. The average length of successful PMAs was 44 months, and our study found the longer the PMA, the higher the success rate. To contrast with non-PHP programs, the top rate for program completion is between is about 45%, depending on the type of program.1
Our return-to-use data is equally impressive. Of 185 participants who signed 198 PMAs, 21 participants, or 12%, had a return to use. In the world of addiction medicine, a 12% return to use rate is remarkable; non-PHP programs average a 40%-60% relapse/return-to-use rate.2
Results from our survey study, in which former participants were asked about the most helpful TMF services in their recovery, will be shared in a separate article at a later date. Overall, former participants cited Accountability, Caduceus support group meetings, and Connections with other clinicians in recovery were among the most helpful aspects of our program.
Conclusion
The TMF participant outcome data is among the best of published data regarding success rates using the PHP model.3,4 Within the next year, we plan to submit this study for publication.
I want to offer a heartfelt congratulations to our TMF participants. The most gratifying aspect of my job is being a part of a TMF participant’s recovery. Having a front-row seat to view and help our participants and their families heal from a horrible, chronic, and lethal disease, and knowing that our participants are providing the best health care they can, is amazing.
The TMF outcome study, together with our participants’ recovery, achievement, productivity, and happiness, confirms that we are on the correct path, protecting patients while saving the lives and careers of Tennessee clinicians, using the best and most effective addiction treatment model available.
References:
1. U.S. Substance Abuse and Mental Health Services Administration (2025), Treatment Episode Data Set (TEDS) 2023: Admissions to and discharges from Substance Use Treatment Services Reported by Single State Agencies. Publication No. PEP25-07-014, 2025. Accessed at https://www.samhsa.gov/data/sites/default/files/reports/rpt56543/2023-teds-annual-report.pdf
2. McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000 Oct 4;284(13):1689-95. doi: 10.1001/jama.284.13.1689. PMID: 11015800.
3. DuPont RL, Compton WM, McLellan AT. Five-Year Recovery: A New Standard for Assessing Effectiveness of Substance Use Disorder Treatment. J Subst Abuse Treat. 2015 Nov;58:1-5. doi: 10.1016/j.jsat.2015.06.024. Epub 2015 Aug 1. PMID: 26277423.
4. Merlo LJ, Campbell MD, Skipper GE, Shea CL, DuPont RL. Outcomes for Physicians With Opioid Dependence Treated Without Agonist Pharmacotherapy in Physician Health Programs. J Subst Abuse Treat. 2016 May;64:47-54. doi: 10.1016/j.jsat.2016.02.004. Epub 2016 Feb 13. PMID: 26971079.